What is the diabetic foot?
Diabetic foot is a condition where the body does not properly control blood sugar levels. It is a common complication of diabetes where the blood vessels and nerves become damaged in your feet and legs. The condition causes numbness, tingling, burning pain, or a loss of feeling in the affected areas. The patient may not be able to sense any injury to their foot until the damage has already been done. If left untreated, the diabetic foot can lead to serious complications including gangrene, amputation, and even death.
Are you familiar with the diabetic foot? If yes, you are not alone. One out of every four adults has diabetes or pre-diabetes. These people can develop something called a diabetic foot. This is one of the most painful complications that come with the disease. For this reason, it is best to know the symptoms and how to get rid of them.
Diabetes as we know is a condition where the body does not properly control blood sugar levels. When the body cannot regulate its glucose level, then diabetes causes damage to the nerves, muscles, skin, and blood vessels. According to WHO estimates, India had approximately 12.4% of the total world’s diabetic population. By 2025, India could become home to about 60% of those with diabetes in Asia.
How do we get a Diabetic foot?
Many reasons cause a diabetic foot. Fungal infections cause 30-40% of diabetic foot wounds. A fungal infection is known as onychomycosis (also referred to as tinea pedis). Fungal infections can lead to ulcers and necrosis of the skin. Diabetes causes the skin to dry out and become susceptible to infection. Poor circulation increases the risk of infection. Also, diabetes changes the immune system making people vulnerable to bacterial infections.
Understanding Diabetic Foot: Diagnosis, Causes, Treatments, Preventions.

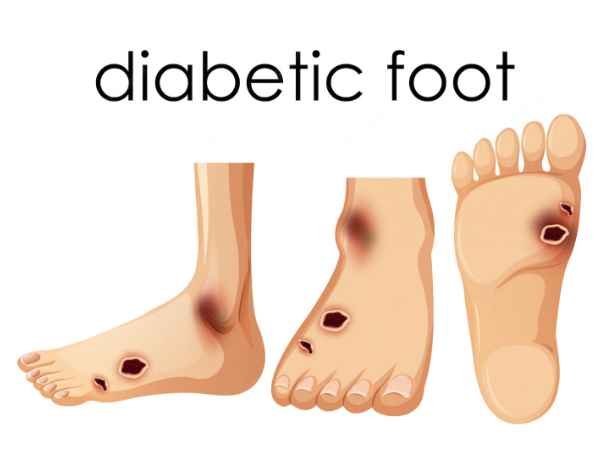
Diagnosis: Diabetic foot is characterized by ulcers and gangrene. The condition is caused by prolonged exposure of the tissues under the diabetic patient’s foot to high blood glucose levels. The ulcers usually start at the base of the great toe and progress upwards towards the ankle.
- A diabetic foot is characterized by tissue damage and infection due to prolonged exposure of the nerves, arteries, veins, and other structures under the patient’s diabetic foot to high blood glucose levels. Diabetic foot usually develops in people with type 1 or type 2 diabetes mellitus. However, in some cases, non-diabetic patients with poor circulation have a diabetic foot.
- Your doctor can diagnose a diabetic foot by examining the ulcers on your feet closely for any evidence of vascular changes, such as white spots or crusted areas on the surface of your skin. He may also perform a nerve conduction study to assess how well your nerves are transmitting pain signals from your feet to your brain.
- Additionally, X-rays may show bone infection in some cases if there is severe bone decay below your injury site. In some severe cases, amputation may be necessary to provide relief from pain and disability caused by a diabetic foot.
Causes: Diabetic foot problems are very common and can severely affect the quality of life of people with diabetes. People with diabetes are prone to developing diabetic foot problems as a result of inadequate blood glucose control. Treating diabetic foot problems early is critical to preventing further complications and minimizing pain. In addition, doctors must work with people with diabetes to prevent and treat any foot ulceration that does occur. Diabetes can affect any part of the body, but it’s most common in Type 1 and Type 2 adults.
Complications: The main complications of diabetic foot problems include ulcers, gangrene, infections, and amputation. In addition, doctors treat these complications with invasive procedures such as amputation.
Signs and Symptoms:

- Symptoms of diabetic foot problems include pain, redness, warmth, and stiffness on the front or back part of the foot. In addition, you may experience difficulty walking or feel extreme pain when your shoes touch the ground or other surfaces. Further symptoms include numbness in the toes, ulcers on the soles of the feet, swelling, and changes in skin coloration.
- Ulcers can be painful and lead to infection; it’s essential to treat all ulcers promptly to prevent gangrene. Diabetes-related complications must be promptly treated to prevent amputation; amputation can result in reduced mobility and disability.
Treatments:
- Doctors treat diabetic foot problems with conventional therapies such as surgery and prescription medications—natural therapies are also effective when used appropriately. Proper treatment for diabetic foot problems includes using both conventional and natural therapies such as compression bandages, rest, and elevation along with oral medications such as antibiotics and painkillers.
- Conventional therapies for diabetic foot problems include compression therapy using compression bandages along with elevation therapy using a boot or special shoe to elevate the feet above the heart level for better blood circulation.
- Doctors have varying opinions regarding natural therapies for treating diabetic foot problems; some caution against taking supplemental supplements because there isn’t sufficient research showing their benefits for diabetics with diabetic foot problems. It’s important to speak with a doctor before incorporating natural therapies into treatment plans for diabetic foot problems since supplement regulations vary by country.
Understanding the Early stages of diabetic foot

- Initial Stage – Blisters or calluses: The first stage of the diabetic foot is known as blisters or calluses. These appear initially at the site where pressure is being applied. In this case, it would be the area between the toes and the shoe. You may notice dry skin that gets red and painful. There could be itching, burning sensation, swelling, and pus formation. Calluses are thickened skin that forms over the bottom of the foot. It generally starts around the heel but can spread across the entire sole. Calluses can become thickened and hardened due to a lack of blood flow. It can also lead to infection if not cared for properly.
- Swelling: Swelling is a symptom that indicates the early stages of diabetes. It looks similar to edema, but it occurs before any pain. It does not cause any discomfort or pain. However, it is considered a warning sign because it means that the foot is becoming uncomfortable and could result in serious complications later on. If left untreated, it may lead to ulcers, infections, amputation, nerve damage, gangrene, or even death.
- Ulcer: An ulcer is a wound caused by trauma to the skin. It is an open sore that exposes the underlying tissue. Common causes include poor circulation, bacterial or fungal infections, excessive friction, and improper footwear. It can occur anywhere on the body including the legs, arms, buttocks, hands, feet, and genitalia. When it happens on the feet, it is called a diabetic foot ulcer. It may look small and shallow, but it carries a heavy burden. It can worsen rapidly, causing severe pain, infection, and even limb loss.
- Infection: Infection refers to the invasion of foreign microorganisms (bacteria) into the body. It is a general term used to describe inflammation caused by bacteria, viruses, fungi, parasitic worms, etc. The infection spreads throughout the body until the affected organs get damaged. A person suffering from chronic infections may experience fever, chills, aches, nausea, vomiting, diarrhea, fatigue, weight loss, and mood changes.
- Gangrene: Gangrene is the final stage of the diabetic foot and it involves the destruction of the extremities resulting in the loss of the affected digit or limb. It can happen anytime after the initial symptoms of the diabetic foot have appeared. It is characterized by softening of tissues and the appearance of blackish discoloration.
Diabetic foot ulcer- What it is, How it happens, Treatment

Diabetic foot ulcers are serious wounds that affect people with diabetes. A diabetic foot ulcer is a compressive disease in which the blood flow to the foot is interrupted. There are two main types of ulcers, aggressive and non-aggressive.
The aggressive type of ulcer is infected and has a high risk of spreading to other parts of the body. People with diabetes have a higher risk of developing an aggressive type of diabetic foot ulcer. Infection can lead to amputation if left untreated. In addition, there is also the non-aggressive type of foot ulcers which are less common but do not pose any health risks. Treating an existing diabetic foot ulcer is essential for maintaining healthy blood flow and preventing complications.
Proper care can prevent diabetic foot ulcers: Effective treatment methods for diabetic foot ulcers include covering, compressing, and prescription drugs such as penicillin or cephalosporin antibiotics for rapid healing. Covering a wound reduces pain from sores by protecting affected areas from external stimuli such as heat, cold, excessive direct sunlight, etc.
Compresses attract pus from wounds and warm it up before applying moist bandages over wounds for deeper cleaning and recovery of wounds. Prescription drugs speed up healing by reducing pain and promoting new cell growth in affected areas via anti-fungal or anti-bacterial agents such as sulfonamides or tetracycline hydrochloride.
People with diabetes should know about their condition so they can take the necessary steps to avoid developing these painful wounds on their feet. Regular checkups with podiatrists help detect early signs of these infections so appropriate treatment can be administered promptly to prevent further complications from developing into serious conditions such as toe amputation or death from gangrene from infected toes.
13 Tips for Diabetic Foot Care: Keep your foot Healthy

- Wear shoes or boots that fit properly. A good pair of walking shoes should have enough room for your toes to move around without feeling cramped. If you’re wearing flip-flops, make sure they don’t cut off circulation to your feet.
- Keep feet dry – wear socks that wick away moisture; use foot powders to help prevent blisters and calluses. Also consider using moisturizing lotions, creams, gels, etc.
- Change out of wet socks at least once per day.
- Check your feet daily for cuts, scrapes, blisters, ingrown nails, and cracks. You may want to apply some sort of protective ointment to these areas.
- Be careful when putting pressure on your feet while sleeping. Try not to sleep directly on top of your feet, and if you do, make sure they are elevated.
- Make sure to trim your toenails regularly. Toenail fungus can spread to your skin and cause sores, itching, and inflammation.
- Don’t walk barefoot. Use slippers or shower shoes instead.
- Have someone else check your feet after a long period of standing or sitting.
- Exercise. Walking, running, jogging, cycling, dancing–anything that gets your heart rate going will benefit your feet.
- Avoid high heels. High heels put pressure on the ball of your foot and can lead to bunions, corns, and hammertoes.
- Avoid tight clothing. Tight clothes can squeeze your feet together and restrict blood flow.
- Take breaks from work and exercise. Your body requires time to heal.
- Wear comfortable shoes. If you spend 8 hours a day in them, your feet need to feel comfortable.
When to contact a doctor for a diabetic foot?
The best time to seek medical attention if you have diabetes foot is when you feel pain, redness, swelling, or any change in the color of your skin. If you notice these symptoms, then you should immediately go to the emergency room. This way, they can examine you and make sure that nothing else is wrong with your body before deciding what treatment plan to use.
Conclusion
Diabetic foot amputations often occur when the patient fails to manage their diabetes, resulting in gangrene, a loss of blood flow to a certain area, and often, the subsequent death of tissue. Diabetics must pay attention to the warning signs of diabetic ulcers so they can seek treatment immediately. The American Diabetes Association (ADA) recommends regular self-checks for neuropathy, nerve damage, and other standard treatments in the event of an ulcer. When treating an ulcer, patients must see a diabetic specialist so they can determine the best course of action.
Thank you for writing this post!
Thank you for writing this article. I appreciate the subject too.